The required rotations during the ONMM2 year depend on the rotations completed during your primary residency. As such, it is at the discretion of the ONMM program director to count previous rotations that are required above. The requirements for the 2 year long ONMM residency must be completed by the end of the residency whether you enter as an ONMM1 or ONMM2 resident.
- The VCOM program requires 1 rotations in each: sports medicine, orthopedics, neurosurgery, rheumatology, neurology, PM&R, pain management / hospice & palliative care, regenerative medicine, and physical therapy
- The more of these musculoskeletal rotations you complete during your primary residency, the more time you can spend on ONMM specific rotations in addition to time spent on OMM continuity clinic & OMM hospital consult service during your ONMM2 training year.
- Rotations completed in a primary pediatric residency with a pediatric focus do count toward the required rotations for eligibility for entry into the ONMM2 level. For example, a resident may complete a pediatric neurology rotation in place of an adult neurology rotation.
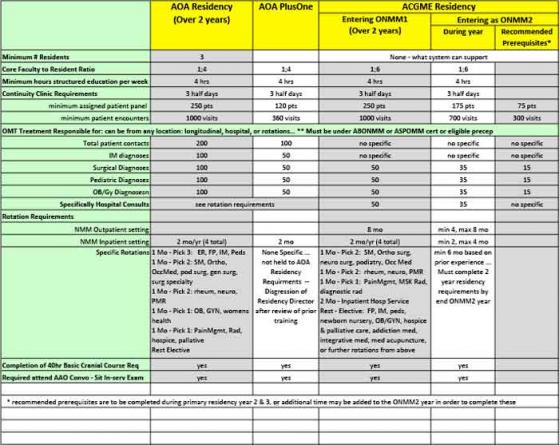
Review Committee for ONMM recommends, though does not require, that a resident have exposure to an osteopathic neuromusculoskeletal medicine clinic, supervised by a neuromusculoskeletal specialist, during his/her primary residency. The Review Committee would recommend the following patient encounters to help prepare a resident for entry into the ONMM2 level of the program:
- a minimum of 300 clinic patient encounters
- a minimum of 75 designated continuity of care clinic panel patient encounters
- a minimum of 15 documented patient contacts with a variety of surgical diagnoses, where an evaluation was completed and osteopathic manipulative treatment was provided
- a minimum of 15 documented patient contacts with a variety of pediatric diagnoses, where an evaluation was completed and osteopathic manipulative treatment was provided
- a minimum of 15 documented patient contacts with a variety of obstetrical and gynecology diagnoses, where an evaluation was completed and osteopathic manipulative treatment was provided
- Clarification:
- A single patient encounter may count toward the 300 required patient encounters; however, that patient would not count toward the resident’s required 75 continuity of care panel patients.
- At the discretion of the ONMM program director, a patient contact may be counted toward the minimum patient contacts for multiple diagnosis (surgical, pediatric, and obstetrics and gynecology)
- At the discretion of the ONMM program director, a clinic patient encounter could count toward the minimum continuity of care patient encounters and toward the minimum patient contacts for patients with a surgical, pediatric, or obstetric and gynecologic diagnosis. The same is true for patient contacts through hospital consultation. Those patient contacts may be counted toward the minimum hospital consultations and toward the minimum patient contacts for patients with a surgical, pediatric, or obstetric and gynecologic diagnosis.
- In order for a resident to include a continuity patient encounter in his/her count toward the minimum 75 designated patients in the continuity of care clinic or the 300 patient care encounters in the continuity clinic, the resident must be supervised by an AOBNMM-certified, AOBSPOMM-certified, or board-eligible attending physician. A supervising physician without such certification or eligibility would not be able to direct a resident to the depth and breadth of knowledge expected of a board-certified physician in the specialty of neuromusculoskeletal medicine.
- Please note, that failure to obtain these recommended hours or some of these rotations prior to entering the ONMM2 year can extend the ONMM2 training year beyond 12 months, and our programs may not be able to accommodate this
- Above is a summary comparison of the AOA & ACGME requirements. Depending on your graduation year and programs accreditation, you will need to be sure you have completed the requirements before graduation of your ONMM residency.
If you have questions regarding your specific completed rotations or future rotations, please submit your questions to:
Melissa Simpkins
Program Coordinator
msimpkins@vcom.vt.edu