Chronic pain affects one in three people worldwide, disrupting work, sleep, relationships and mental well-being. For many individuals, traditional treatments fail to fully address such pain. To respond to this need, a group of researchers and clinicians at Auburn campus of the Edward Via College of Osteopathic Medicine (VCOM), known as the Pain Free Research Collaborative, are leading an innovative effort to rethink how chronic pain is understood and treated. The collaborative is led by William G. Pearson, Jr., PhD, discipline chair, and associate professor of anatomical sciences at VCOM-Auburn. Their approach draws upon osteopathic principles and emerging neuroscience.
Beyond Pills and Protocols
Historically, chronic pain treatment has relied heavily on medications, including opioids, with varying levels of success and significant associated risks. While medications can provide short-term relief, they are not designed to address the complex interaction between mind, body, and lived experience that shapes how individuals cope with pain. Osteopathic philosophy emphasizes the body’s capacity for self-healing and the importance of treating the whole person. This framework may provide new ways of thinking about patient care in the context of chronic pain.
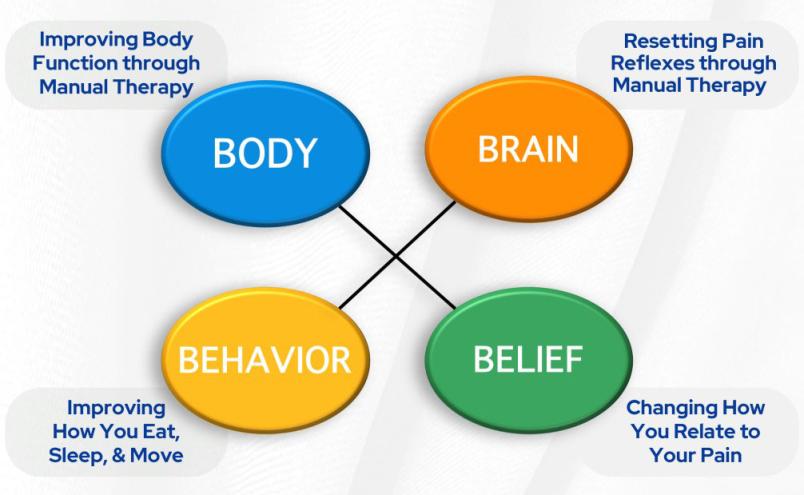
Researchers at VCOM are exploring a treatment path that integrates neuroscience, trauma-informed care, and lifestyle medicine. This approach, termed Compassionate Integration, brings together multiple specialties to address not only symptoms but also the root causes of pain. Instead of applying one-size-fits-all treatments, patients receive individualized support from a team that may include osteopathic physicians, psychologists, lifestyle coaches and neurologically informed practitioners.
A Pilot Study in Compassionate Integration
The Pain Free Research Collaborative is currently conducting a pilot longitudinal observational study. This preliminary research is an important first step toward larger clinical trials. The study follows patients over time to evaluate how the Compassionate Integration model influences pain, functional ability and overall well-being.
Participants are introduced to a range of non-pharmacological interventions. Some individuals receive osteopathic manipulative treatment (OMT) and dry needling, which are hands-on therapies that address physical tension and structural imbalances. Others participate in autonomic recalibration, a neuroscience-based technique designed to calm the nervous system and reduce sympathetic overdrive. Counseling and pain education are also provided to help participants reframe maladaptive thoughts, process trauma and build resilience. Nutrition guidance and personalized lifestyle coaching further support long-term healing.
Each participant determines which interventions to engage in, and many choose multiple options. This flexibility mirrors real-world healing, where various approaches often interact to produce lasting outcomes.
The research team is particularly interested in how factors such as early-life trauma or pain-related beliefs affect an individual’s response to treatment. By examining these variables alongside clinical outcomes, the investigators aim to better understand why certain interventions are more effective for some patients than for others.
Looking Inside the Brain
A subset of participants in the pilot will undergo functional magnetic resonance imaging (fMRI) to investigate how chronic pain, and its treatment affects neural networks shaped by trauma and autonomic drivers of pain. Researchers are evaluating whether interventions such as autonomic recalibration can restore healthier patterns of brain connectivity and whether these neural changes correspond with meaningful reductions in pain. This work is conducted in collaboration with MRI specialists at Auburn University, under the guidance of Dr. Pearson.
Building Toward the Future
At the center of this research is a student–participant partnership model. Each participant is paired with a dedicated VCOM-Auburn student who accompanies them throughout their care journey. Students provide a consistent point of contact, facilitate communication across disciplines, coordinate clinical visits and support participants in reflecting on their progress. For the students, this experience is formative in developing the habits and skills required to become compassionate physicians.
The pilot study is also laying the foundation for a larger, externally funded clinical trial utilizing an advanced research design known as a Sequential Multiple Assignment Randomized Trial (SMART). Even at this early stage, the research is focused not merely on data collection but on producing meaningful improvements in participants’ lives.